By Natalie
A large proportion of the women who come to see me for Abdominal-Sacral massage or to my ‘Womb Wise’ workshops, are experiencing menstrual health challenges, digestive issues and/or are wanting support with their fertility. Regardless of why they come, I always ask a number of questions about their menstrual cycle, past or present. This is because the health and length of the menstrual cycle and the quality and quantity of blood at each period gives valuable information about our overall health and often gives clues as to what may be contributing to difficult symptoms and health challenges.
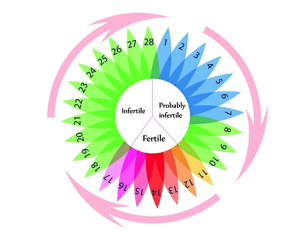
Whilst most women can describe their period and approximate cycle length, many are not sure exactly when they ovulate (release an egg from their ovaries) or if this is happening every cycle. Often it is assumed that ovulation occurs on day 14 because that is what is taught in schools. However, even if you have a ‘textbook’ 28/29-day cycle this may not be the case for you. Knowing when you ovulate is not only important information when trying to conceive, it also gives valuable information about your hormonal balance and is a real advantage for contraceptive purposes, as there is only a 7 day window each month when conception is actually possible.
The reason the fertile window is around 7 days long is because sperm can live for 3-5 days so if intercourse occurs up to 5 days before ovulation, conception is still possible. Then we have to take into account that an egg can live and be fertilised for approximately 12 hours after it is released, (up to 24 hours). So depending on when intercourse occurs and the time of day the egg is released, this gives us a potential ‘fertile window’ of 5 days before ovulation, the day of ovulation itself and 1 day afterwards. The right environment needs to be in place for sperm to survive however, so for some women the window is shorter. For contraceptive purposes, extra precaution is recommended 6 days prior to ovulation and for 3 days afterwards.
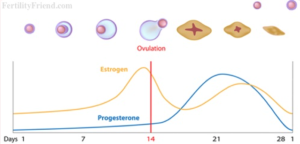
Another valuable aspect of knowing when you ovulate is that ovulation occurs in the middle of two distinct halves of the menstrual cycle and the length of each half can illuminate the health and balance of two important hormones, oestrogen and progesterone. The first half, from day 1 of the period (when the proper flow of blood begins) up until ovulation, is called the Follicular phase. During this phase new follicles are developing in the ovary, each containing an egg and the dominant follicle will release its egg at ovulation. Whilst they are developing, the follicles also produce oestrogen, which rebuilds the womb lining and is important for creating fertile cervical conditions to aid conception. When in balance, oestrogen is a wonderful hormone that helps us to feel confident and to have energy and libido. It also promotes healthy hair and skin and the production of the feel-good neurotransmitter serotonin.
Image credit: www.FertilityFriend.com
To allow enough time for the follicles to develop properly and for a nice healthy womb lining to develop the Follicular phase needs to be at least 11 days long, typically 14 days but it can often be longer. This phase of the cycle is very sensitive to stress and hormone fluctuations, whether that is from internal or external sources, which can cause it to vary in length for any given woman. However, apart from during stressful times or significant lifestyle changes such as travel, it should stay more or less the same number of days, month-to-month.
The second half of the cycle is counted from ovulation to the onset of the next period and is called the Luteal phase. It has this name because when the dominant follicle releases its egg at ovulation, the remaining tissue of that follicle transforms into what is know as the Corpus Luteum. The Corpus Luteum has a very important role in that it starts to produce increasing amounts of progesterone, our pro-gestation hormone. This hormone nourishes the womb lining and keeps it in place ready to receive an embryo, should conception occur. It also raises our BBT (Basal Body Temperature) to create the optimal conditions for implantation of an embryo. Progesterone is a bit like Nature’s Valium in that when it is in balance and in sufficient quantity, it has a gentle calming effect on the body in this phase of the cycle. It is also a natural diuretic and helps stabalise the blood sugar. When levels of progesterone are low however, or are being overpowered by oestrogen, it will be reflected in the cycle in a myriad of ways, such as uncomfortable symptoms or compromised fertility.
At the end of the luteal phase, if pregnancy has not occurred the Corpus Luteum ceases to function, progesterone levels plummet along with oestrogen and the womb lining sheds resulting in a period and the beginning of a new cycle. However, if an egg has been successfully fertilised and has embedded itself well in the womb lining, the Corpus Luteum will continue to produce progesterone until the placenta takes over towards the end of the first trimester of pregnancy.
Whereas the Follicular phase varies woman-to-woman, and sometimes month-to-month, the Luteal phase should not fluctuate and is commonly 14 days long, (maximum 16 days). This is because the life span of the Corpus Luteum is on average 12-14 days. If this phase of the cycle is longer than 16 days, it suggests pregnancy or that ovulation did not occur when it was thought to have. This can be the case with conditions such as PCOS, when the body may attempt to ovulate a number of times before being successful. These attempts to ovulate may be picked up on ovulation kits but we need other tools to confirm that ovulation did actually occur. A period (with a flow of blood as opposed to spotting) is a good sign ovulation occurred and you can then count back around 14 days from that and start to get a sense of which day you likely ovulate each month.
If the Luteal phase is consistently 10 days or less, it suggests something called a ‘Luteal Phase Defect’. This can compromise fertility, as there is not enough time for the egg released at ovulation to be fertilised and to safely implant before the womb lining is shed with a period. Knowing when ovulation occurs allows the shortening of this phase to be picked up sooner rather than later and measures can then be taken to correct it.
So how do you tell when ovulation occurs?
Some women feel ovulation as a twinge on one side of the lower abdomen corresponding to the side that ovulation is occurring. There can also be some general discomfort in the lower abdomen for a few hours and sometimes a little spotting. However, if there is consistently significant pain mid-cycle or persistent spotting, it is important to get it checked by the GP as sometimes it can be due to ovarian cysts or other conditions. Just as an aside, it is a myth that the ovaries alternate right, left, right, left each cycle, it is in fact more random although it can follow that pattern.
Charting your BBT (Basal Body Temperature) each month is another way to tell when ovulation occurs. This being said, until you have been charting for a few months, monitoring your temperature is less helpful at determining when ovulation will happen. It is however an effective way to confirm ovulation has occurred. When charting, you may note that your temperature dips just prior to ovulation but this is not always noted. What you will see however is that your BBT will rise over the next 1-4 days (ideally 1-2 days) following ovulation. The temperature should then remain high for the rest of the cycle, coming down a day or two before the next period. Once three consecutive upper range temperatures have been noted after ovulation it is safe to assume that ovulation has occurred and that your fertile window is over. (Unless of course there are other factors contributing to a raised temperature such as fever or illness.) In order to accurately chart your BBT you do need a digital thermometer showing tenths of a degree.
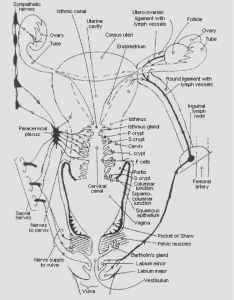
Another change that occurs during the ‘fertile window’ that helps us to predict ovulation is the position of the cervix. During most of the cycle the cervix remains low, closed and sealed, blocking the access of sperm. However, as ovulation approaches the cervix moves up higher in the vagina and opens ready to receive sperm. For these days before ovulation the cervical crypts of the cervix also secrete a slippery alkaline fluid/mucus to aid conception.
Image credit: Erik Odeblad, Ovulation Method Research and Reference Centre of Australia.
Awareness of changes in the cervical secretions and the arrival of this slippery wet fluid is a valuable predictive sign that ovulation is approaching. Some women are more aware of this than others as there are a number of factors that affect the quality and quantity of this ‘fertile’ cervical fluid. Long-term use of the hormonal Birth Control for example, can dry up the cervical secretions. This is worth being aware of if you wish to conceive and are using something like the Pill, so that you can come off it well in advance of trying to conceive. This gives your body time to re-establish necessary amounts of cervical fluid to enable conception to occur.
So what changes in cervical fluid might you notice?
After the period ends there is typically, although not always, a few ‘dry days’, when there is no noticeable cervical secretions, or it might be pasty. However, as ovulation approaches and the follicles within the ovary produce increasing amounts of oestrogen this cervical fluid changes in appearance and quantity. The significance of this is that outside of the ‘fertile window’ the cervical fluid is thick and appears mesh-like under a microscope and will block sperm. However, as ovulation approaches this fluid becomes wetter and more slippery, akin to egg white and contains within it channels that act like an escalator to the sperm, helping them get swiftly to the egg released at ovulation. This wetter cervical fluid is also alkaline, protecting the sperm from the otherwise hostile PH of the vagina. It also provides the sperm with glucose and other nutrients to help them on their journey to the egg.
The peak day of this cervical fluid (when we notice the most) is usually the day of or the day before ovulation when you may notice what feels a bit like the beginning of a period except the fluid is cold, not warm like blood and the cervical fluid is stretchy and clear. After ovulation there is a noticeable absence of this slippery, wet fluid and if anything is noted at all it is pasty or drier in consistency. If it were looked at under a microscope it would show the mesh-like, sperm-blocking structure once again. For the rest of the cycle, any secretions noted are thicker or drier and for many women they won’t notice anything further until their next period. Without the slippery, wet, alkaline fluid sperm cannot survive very long and have no assistance in reaching the egg in time.
The combination of charting both BBT and the changes in cervical fluid, is a very good way to begin to know your cycle, to pin point ovulation and to determine your ‘fertile window’. We have seen too that knowing when you ovulate sheds light on the relative lengths and health of the follicular and luteal phases of the cycle, giving valuable information about the balance of oestrogen and progesterone. As mentioned above, an imbalance in the ratio of these hormones plays a significant role in many menstrual health and fertility challenges. If ovulation is not occurring each month, or not occurring at all it is important to know this as without regular ovulation optimal amounts of oestrogen and progesterone are not made, which has wide reaching effects on both health and metabolism.
As women approach menopause it is not uncommon to begin to notice anovulatory cycles (cycles without ovulation) but in this age group it is not abnormal and can occur more frequently as the hormone levels naturally change with age. However, aside from this or during pregnancy women ideally want to be ovulating every month to reap the benefits of healthy balanced hormones. Getting to know your own unique cycle enables you to be the first one to notice if anything changes in your cycle and also helps you to choose the best course of action to take to find greater hormonal balance, optimal fertility and health. It is empowering knowledge enabling you to be your own health detective and to tune into the messages given by your body.
One final thing to note is that hormonal birth control, such as The Pill, works by shutting down ovulation and the production of our own endogenous hormones and as a result the monthly bleed that occurs is not a true period but a chemically induced withdrawal bleed, timed by the manufacturers to mimic an average menstrual cycle. The synthetic forms of oestrogen and progesterone provided by the pill also have very different effects in the body than our own hormones have. If you are on hormonal birth control, the suggestions made above for charting the cycle will therefore not be relevant, as you will not be ovulating.
In part two of this blog post, I will share the basic steps to charting your cycle.
Visit our Women’s Health Page for further information about how our Alma Vale Centre therapists can support you in optimising your health.
You can also read more blogs about fertility here.